Overactive Bladder
Brief Overview: Syndrome consisting of symptoms of urinary urgency with or without incontinence, frequency, and nocturia in the absence of other identified conditions.
Prevalence: 16% of men and women >40. 30-40% of men and women >75. Higher incidence in females, and Caucasians.
Etiology: Not well understood. Detrusor overactivity is found in some patients. A combination of various mechanisms can contribute- hormones, neurogenic, myogenic, and pharmacologic.
Risk Factors: Neurogenic- stroke, Parkinson's, MS, spinal cord injury. Diabetes, depression, aging, outflow obstruction, increased BMI, high caffeine intake, smoking
Commonly Associated Conditions: Pelvic floor disorders, IBS, depression/anxiety, DM, ADHD, obesity
Common Symptoms: Urgency is a primary symptom. Urinary frequency, leakage/incontinence, nocturia.
Pertinent History:
- Voiding diary quantifying frequency/nocturia/pad use
- Any prior medications/therapies utilized and treatment response
- Constipation/diarrhea/fecal incontinence
- Prior pelvic surgeries- prolapse, hysterectomy, radiation, prior incontinence surgeries
- Medications-diuretics, prescription/OTC
- Menopause/hormone replacement
Physical Findings and Exam: Mental status/cognition, pelvic exam to evaluate for pelvic organ prolapse, pelvic floor tone, masses/tenderness, condition of vaginal mucosa for atrophy, inflammation, cough stress test for stress incontinence
Common Labs, Imaging, and Tests: UA C&S r/o infection. No other diagnostics are indicated for diagnosis, history and exam are sufficient.
Common Treatments and Medications:
- 1st Line:
- Lifestyle modification- weight loss, reduce caffeine/alcohol/nicotine, bladder retraining, and toileting schedules
- keeping bladder diaries for ongoing evaluation and treatment responses.
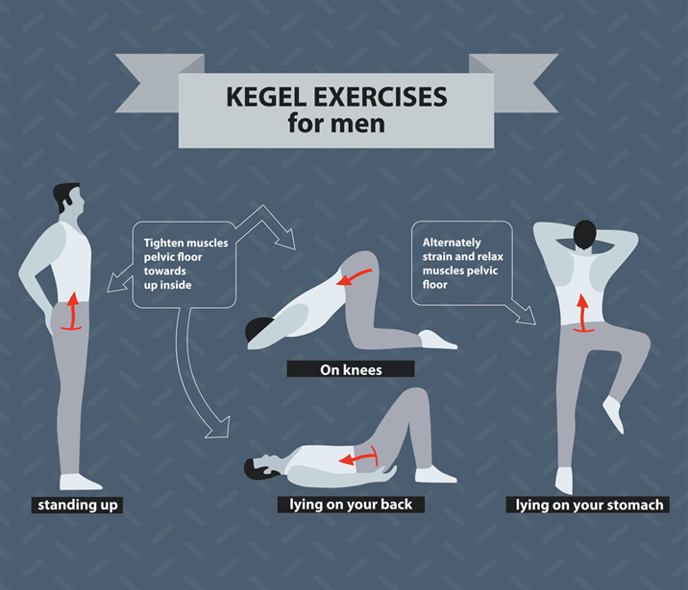
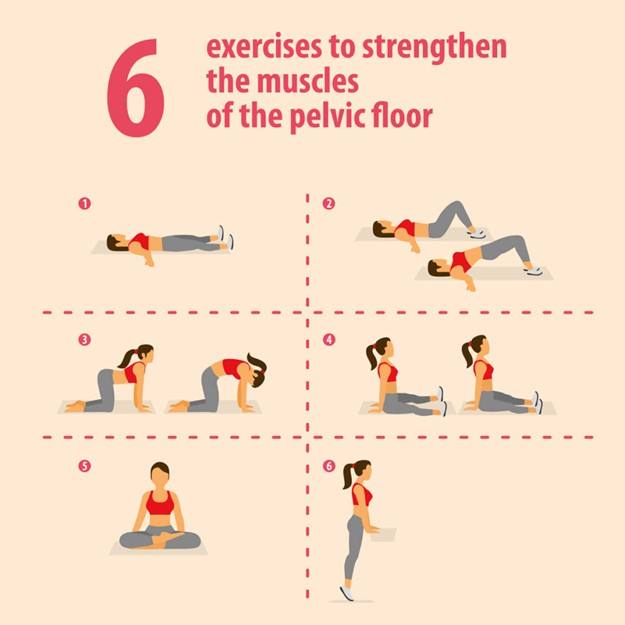
- Pelvic floor physiotherapy including biofeedback, vaginal weights, electrical stimulation, and kegel exercises.
- 2nd Line- Medications:
- Antimuscarinics/anticholinergics- tolterodine (2-4mg/d), trospium XR (60mg/d), darifenacin (7.5-20mg/d), solifenacin (5-10mg/d), oxybutynin IR/ER(5-20mg/d), fesoterodine (4-8mg/d). These are high-risk medications in the elderly and common side effects are dry mouth, dry eye, and constipation. Risk of cognitive changes with long-term use.
- Beta adrenergic agonist-promotes detrusor relaxation- mirabegron/Myrbetriq (25-50mg/d), Gemtesa* no generic (75mg/d). Myrbetriq can cause a rise in BP, not uncommon to see cardiology d/c this medication. Gemtesa is usually very well tolerated but $$$.
- 3rd Line:
- Tibial nerve stimulation, office-based therapy requiring weekly sessions over 3-4mo and periodically thereafter
- Sacral neuromodulation- Axonics/Interstim- implanted neurostimulator of sacral nerves, modulates activity of bladder, sphincter, pelvic floor muscles. Also indicated for fecal urgency/incontinence. Newer models/operating systems have longer battery life and MRI compatibility. Older models are not MRI-compatible, and need to be directed to clinic/rep if questions regarding their personal device. Older models often require recharging their devices. Both systems have devices to make adjustments on their therapy.
- Intravesical botulinum toxin- Botox. Chemical denervation promoting the relaxation of the bladder. Requires retreatment q4-12 mo on average. The biggest risk with this procedure is retention.
Potential Complications and Contraindications: n/a. The main concern is the impact on quality of life. Older adults may seclude themselves for fear of embarrassment.
General Health and Lifestyle Guidance: Attention to skin care if using incontinence pads/appliances such as Purewick etc to avoid skin breakdown. Avoid caffeine and alcohol and encourage adequate hydration. Manage comorbidities such as diabetes and hypertension. Routine exercise for core/pelvic floor strength. Monitor weight, manage obesity, and weight loss for increased BMI.
Suggested Questions to Ask Patients:
- Are you taking your prescribed medications? Are you experiencing any side effects from these medications?
- If botox- do you feel that you are able to empty your bladder?
- If SNM- are you able to adjust your device yourself? Have you contacted the clinic and/or rep for concerns regarding your device?
- How many servings of caffeine/alcohol are you consuming daily? Can you decrease or eliminate them?
- How many servings of water are you consuming daily? *Many people will avoid hydrating for fear of worsening symptoms*
- Understand that comorbidities such as DM, HTN, and CHF may use medications that will worsen OAB symptoms. They must not stop those medications without approval by PCP/cardiology.
- Discuss Pelvic Floor PT and share common exercises.
- Depression screening if symptoms interfere with QOL.

![MCP-1.png]](https://resources.mycarecoordinator.com/hs-fs/hubfs/Logos/MyCare%20Program%20Logos/MyCare%20Program/MCP-1.png?height=50&name=MCP-1.png)